Clean claims, confident scores, measurable savings
Take control of risk adjustment with AI-powered analytics that validate diagnosis coding, reduce audit exposure, and protect revenue before the claim is paid.
When diagnosis codes don’t match the care, your plan pays the price.
Inaccurate HCC coding drives billions in improper payments and exposes health plans to audits, penalties, and lost revenue. Whether it’s unsupported diagnoses or misused quality codes, plans must ensure coding accuracy at scale before regulators find the errors.
Discover the Power Behind Our AI Tools
Validate every diagnosis. Protect every dollar.
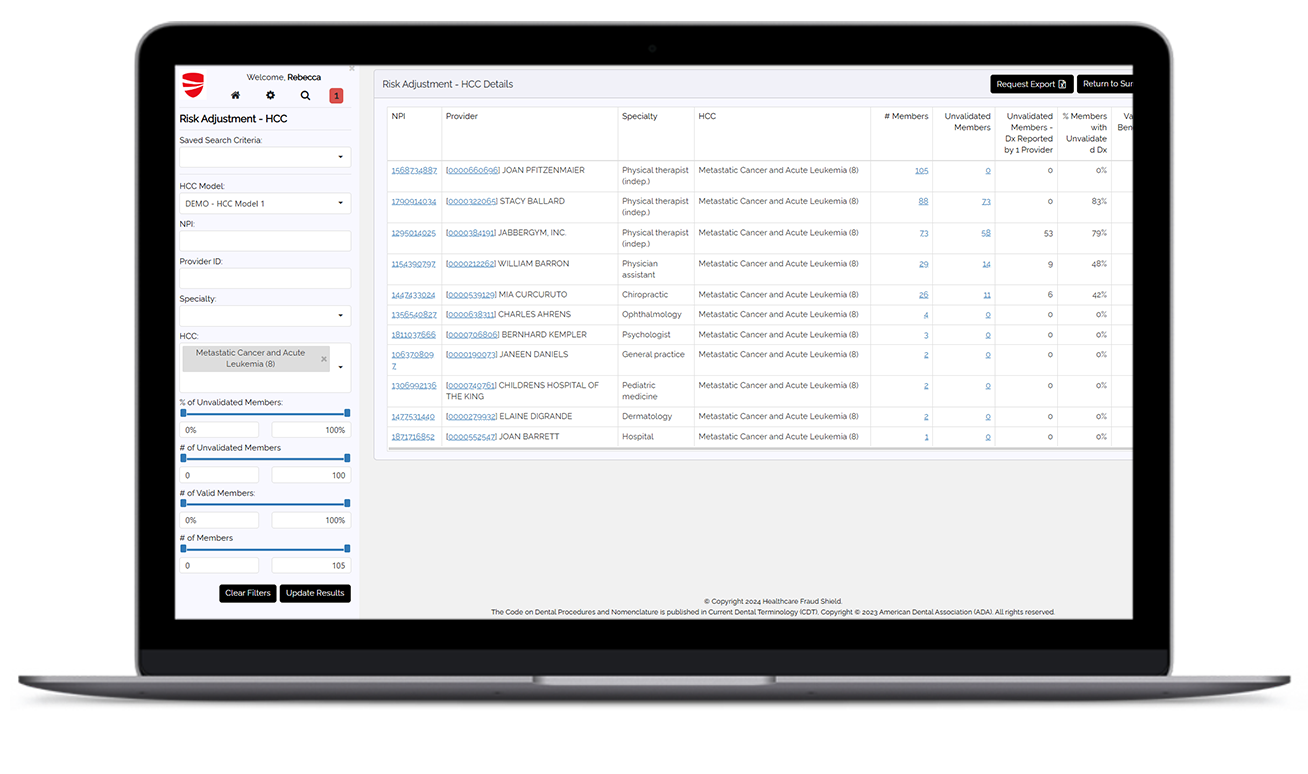
Detect Upcoding & Unsupported HCCs
AI-powered analytics identify diagnosis codes that lack clinical support, helping reduce overpayments and inappropriate risk scores.
Validate Diagnoses Across the Care Journey
The system cross-checks HCC codes with treatment history, prescriptions, and utilization data to ensure accuracy and plausibility.
Reduce Audit Risk Proactively
It flags unsupported or inconsistent coding patterns before claims are submitted, helping plans avoid CMS and state-level penalties.
Improve Quality Score Integrity
By identifying misused quality measure codes, the solution helps restore accurate reporting and strengthens performance metrics.
Drive Smarter Audits & Education
It delivers targeted, actionable insights that enable focused audits and support provider education on correct coding practices.
Integrate with Broader FWAE Strategies
Fully embedded in the HCFSPlatform, RiskAdjustment™ connects seamlessly with pre-payment review, case management, and more.
Download the Complete RiskAdjustment™ Product Overview
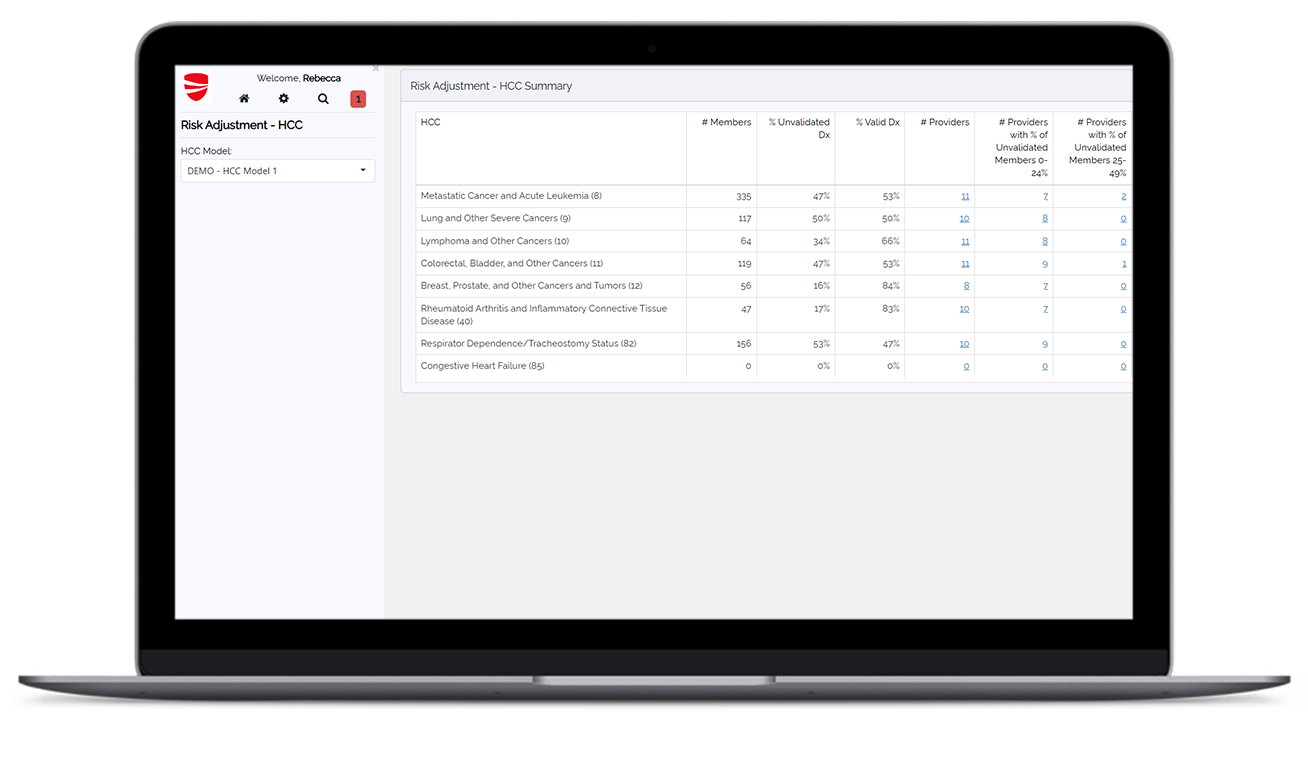
Better insights mean fewer errors, less risk, and measurable ROI.
Decide with confidence.
